Michael P Lebowitz D.C.
Noah D Lebowitz
Michael Lebowitz
2550 I Road
Grand Junction, CO 81505
970-623-9565
Noach2343@aol.com
Hypercoagulation Disorders, a PAK Approach
Abstract
Hypercoagulation is a condition that in extreme
cases can lead to a deep vein thrombus, pulmonary emboli, and stroke. In less
severe cases it has shown to be associated with chronic fatigue, fibromyalgia,
nutrient deficiency, etc. Using Professional Applied Kinesiology the authors
have developed a technique to possibly check for a patient being in a
hypercoagulation state. This allows us to help the patient decrease their
chance of a serious circulatory incident, or resolve chronic health issues that
haven’t yet been resolved.
Keywords:
Hypercoagulation, deep
vein thrombosis, thrombus, stroke, pulmonary embolism, chronic fatigue
Introduction/Background
Hypercoagulation is a condition manifesting in increased
fibrin in ones blood and as a result the individual is at an increased risk of
developing a thrombus (blood clot). If a person goes too far into a hypercoagulative state they develop deep vein thrombosis
(DVT) which can be broken up and lead to pulmonary embolisms (PE), a myocardial
infarction (MI), or stroke.
According to research done by David Berg, in less
severe cases hypercoagulation can lead to chronic fatigue, fibromyalgia, and
osteonecrosis. [1]
Checking for hyper-coagulation has never been
attempted before in Professional Applied Kinesiology (PAK), even though it is a
leading cause of illness in the United States. It is estimated that
300,000-600,000 suffer from a DVT in the United States each year, and that
60,000-100,000 die from a DVT or (PE) each year. [2] Well known people such as
Hilary Clinton, Mariano Rivera, and Serena Williams are several of many that
have suffered recently from blood clots, leading to an increased public
awareness.
Hypercoagulation can be caused by a myriad of issues
including: infections, metal and chemical toxicity, immobility, surgery,
supplemental estrogen, malignancy, genetics, or prolonged periods of time spent
at very high elevation.
Research done by Dr. Pryzdial
from the Centre for Blood Research shows how certain viruses, such as herpes
simplex (HHV6, EBV) or cytomegalovirus (CMV) “express phosphatidylserine
like procoagulant activity, capable of binding Xa and Va to form the prothrombinase complex.” [3] David Berg went on to note
that 70% of patients studied with Chronic Fatigue Syndrome as well as Multiple
Sclerosis were infected with HHV6 [4]. HHV6 is known to reside in endothelial
cells, causing them to lose their ability to synthesize prostacyclin, and thus
have a decreased ability to deter platelet adhesion. [5] Berg also mentions how
the hypercoagulative state found in patients with
chronic fatigue syndrome and fibromyalgia does not result in a thrombis, though is still problematic. While a thrombis was
not formed, fibrin deposition in blood vessels can lead to hypoxia, nutrient
deficiency, and a plethora of other symptoms.
By screening ones patients for hypercoagulation and giving them supplementation and lifestyle changes, one could decrease the risk of the patient developing a DVT or PE. Also by thinning out one with “thick blood” it will allow the patient to more efficiently deliver oxygen and nutrients to all parts of the body, which may have currently obstructed pathways. By doing this one can help chronic patients with conditions such as chronic fatigue, fibromyalgia, nutrient deficiencies, etc.
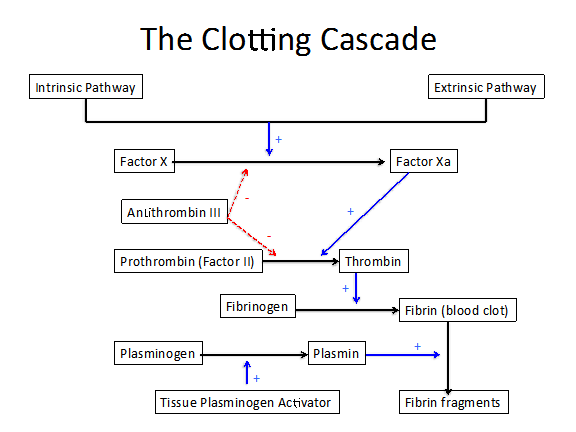
While the clotting pathway is quite complicated, we
chose to focus on four main pro-coagulative factors and four main
anti-coagulative factors.
Pro-coagulation
Factors:
S Prothrombin/Coagulation
Factor II
An inactive protein
synthesized by the liver and released into the blood, which is then converted
to active thrombin in the process of blood clotting.
S Thrombin
The active enzyme
produced from Prothrombin, which acts to covert fibrinogen to fibrin.
S Fibrinogen
Another inactive
clotting factor in blood plasma that is converted to fibrin. Produced by liver and
plasma cells, fibrinogen accounts for approximately 7% of blood plasma
proteins.
S Fibrin
The final step
in the clotting cascade. Fibrin is insoluble, essential to blood clotting, and
formed from fibrinogen by the action of thrombin.
Anti-coagulation
Factors:
S Antithrombin
III
An
anti-coagulant, it blocks action of pro-clotting agents (factors XII, XI, IX, X
and II).
S Plasminogen
The inactive
enzyme precursor of plasmin.
S Plasmin
An enzyme
present in blood that degrades many blood plasma proteins, most notably, fibrin
clots. It activates collagenases, some mediators of the complement system, and
weakens the wall of the Graafian follicle (leading to
ovulation).
S Tissue
Plasminogen Activator / tPA / PLAT
A protein
involved in the breakdown of blood clots. As an enzyme, tPA catalyzes the conversion of plasminogen to
plasmin. Because it works on the clotting system, tPA is used in clinical medicine to treat only
embolic or thrombotic stroke. Use is contraindicated in hemorrhagic stroke and
head trauma.
A person wants to have adequate pro-coagulation
factors as well as anti-coagulation factors to be in proper balance for optimum
body function. Just as being in a hypercoagulative
state is dangerous, being in a hypo-coagulation state can be a serious health
concern. If ones blood does not clot properly, a person can experience
increased bruising, and the potential for excessive internal or external
bleeding, such as someone suffering from hemophilia would experience.
When checking for adequate amounts of clotting
factors in the blood via muscle testing they should neither inhibit a
facilitated muscle, nor facilitate an inhibited muscle, unless something is
abnormal, just as would occur in food or nutrient testing. Using PAK we can not
only check for if the person has a coagulation issue, but also see if it is
with clot production or clot breakdown.
The question may arise of what to do once such
problems have been discovered. There are many natural substances that are known
and have been used for centuries to thin the blood:
1. Ginkgo Biloba
is one such which has been shown to be a potent antagonist of platelet
activating factor, decreasing clot formation.
2. Ginger has been shown to have blood-thinning
properties. [6] Current research out of
the University of Sydney showed ginger to inhibit arachadonic acid induced
platelet aggregation via inhibition of the COX-1 gene. [7] New studies claim
ginger to be a more potent anti-coagulative than aspirin.
3. Pomegranate Juice has been shown
to also inhibit platelet aggregation, thus helping to deal with
hyper-coagulation. [8]
4. Green Papaya has been shown to increase
fibrinolysis and the break down of already formed clots. [9]
5. Bromelain, found in fresh
pineapple, has been shown to decrease blood coagulation by several
pathways. Bromelain acts by inhibiting
the generation of bradykinin at the inflammatory site via depletion of the
plasma kallikrein system. It also limits the formation of fibrin (clots) by
reduction of clotting cascade intermediates. [10] Bromelain has also been shown
in multiple studies to stimulate the conversion of plasminogen to plasmin, resulting
in increased fibrinolysis (dissolution of clots/fibrin). This combination of
effects can make it very useful in people with hypercoagulation tendencies.
[11].
6. Nattokinase can be found in
supplemental form or in natto as a food and has been
shown to decrease coagulation in the blood by decreasing plasma levels of
fibrinogen, as well as pro-coagulation factors VII and VIII. [12] It has also
been shown to increase plasma levels of tPA,
thus increasing fibrinolytic activity and lysis of
thrombi. [13]
7. Shochu
(Japan) / Soju (Korean) is known to increase urokinase-like plasminogen activator, leading to
fibrinolysis, at the highest rate among all types of liquor; and is routinely
in Japan for cardiac health. [14]
Chapman Reflexes have been used in PAK to help
stimulate the function of organ systems of the body. The authors have found a
Chapman-like reflex that seems to negate a positive test for hypercoagulation
in a high percentage of cases. The reflex is bilaterally located on the anterolateral
portion of the neck over the carotid artery where the baroreceptors are found
at the carotid bifurcation (approximately C4).
Procedure
All patients with any of the conditions previously
mentioned (stroke, DVT, fibromyalgia, miscarriage history, etc.) or a family
history of any of these, should be automatically checked for a clotting
disorder. For patients without these symptoms, a quick and effective pre-screen
has been developed to see if further testing is necessary. As a potential
“pre-screen” to see if a patient should be checked for a coagulation issue, the
authors have noticed that when testing a facilitated muscle (i.e. pec major clavicular) you can
squeeze the patients distal forearm firmly, decreasing circulation for
approximately 10 seconds, and then re-test the patient while still squeezing.
If the previously facilitated muscle is now inhibited, the patient should be
checked for having a hyper-coagulation disorder as described below. This test
doesn’t correlate 100% with an abnormal test for hypercoagulation but appears
to be positive in most of the cases (there can be false positives due to
forearm injuries, etc.). If you suspect the disorder but the patient passes the
“squeeze test”, we would still recommend testing further as described next.
1. See if any of the following
pro-coagulative vials inhibits a facilitated indicator muscle: Thrombin,
Prothrombin Factor II, Fibrinogen, & Fibrin. If any of them weaken, it is a
positive test.
2. See if any of the following
anti-coagulative vials facilitate an inhibited muscle: Antithrombin III,
Plasmin, Plasminogen, & Tissue Plasminogen Activator. If it does, it is a
positive test.
3. See if a mixture of
anti-coagulant encouraging herbs (HemoGuard Supreme
1-800-922-1744) as previously mentioned negates the positive test.
4. If severe, also consider adding
systemic enzymes like nattokinase and earthworm-derived enzymes to the products
in step 3. If you do, warn the patient of potential bruising from taking too
large of a dose.
5. Other helpful measures include:
Eating
raw pineapple as a snack away from other foods
Drinking one ounce of Shochu or Shoju daily with or
without food
6. These findings (positive tests
in step 1 and/or 2) are much more common when family history includes, strokes,
heart attacks, clots, embolisms, or miscarriages. They are also aggravated by
taking estrogen, having an infection (chronic or acute), lack of exercise,
dehydration, surgery etc.
7. After identifying
supplementation to negate the positive hypercoagulation reflex, see if light
pressure on the carotid baroreceptors negates the positive test. If so apply
light pressure rubbing over the spot for 10-20 seconds while the patient is
exposed to the factors that showed positive. Re-test the vials, and they should
show up negative.
8. Recheck the patient in a month.
If the tests are now negative see if the supplements still strengthen a weak
indicator muscle. If they do, continue with supplementation. If not just advise
the patient to continue pineapple, shochu etc.
9. CoQ10 can
increase coagulation and supplementation containing it should be discouraged in
these type of patients.
10. If the patient is already on pharmaceutical anti-coagulants it is
not advisable to supplement further as it can
increase the risk of bleeding
disorders. The authors though have seen many people on these medications that
still
fail
the above PAK screening test and they fell are still at risk. If you are not
licensed to prescribe it is difficult to make any recommendations in these
cases.
The above procedure can be reversed checking a
patient for hypo-coagulation.
1. See if any of
the following pro-coagulative vials facilitate an inhibited indicator muscle:
Thrombin, Prothrombin Factor II,
Fibrinogen, & Fibrin. If any of them
strengthen,
it is a positive test.
2. See if any of the following
anti-coagulative vials inhibit a facilitated indicator muscle: Antithrombin
III, Plasmin, Plasminogen, & Tissue Plasminogen Activator. If it does, it
is a positive test.
Discussion
While
working with this technique for the past year we have found that most people
with family histories of coagulation abnormalities, strokes, miscarriages, etc-
will test positive on at least one of the above screening tests and often times
many of them. Using the therapies outlined above most often lead to a return to
normal testing within a month’s time. While we cannot be positive what we are
accomplishing we think we are making a positive impact on returning the person
to a normal state of coagulation and thus helping prevent potentially lethal
events in their future health.
There are many lab tests that check for genetic
tendencies to hypercoagulate and much controversy
exists on interpretation, strategies etc. The recommendations above come from
the personal research of one of the above authors who almost died from massive
pulmonary embolisms secondary to a West Nile Virus infection in 2011.
Conclusion
Screening for hypercoagulation is a quick and
easy test that may potentially be life saving for your patients. It is well
worth the minute or two it takes and it may help also aid in resolution of certain
unresolved symptoms in the chronic patient.
References:
1. Berg D, Berg LH, Couvaras J, Harrison H. Chronic fatigue syndrome &/or
fibromyalgia as a variation of antiphospholipid
antibody syndrome (APS): An explanatory model and approach to laboratory
diagnosis. Blood Coagulation and Fibrinolysis 1999: 10 435-438.
2. "For
Patients." Get Involved. UNC Blood Clot
Research Program, n.d. Web. 07 Jan. 2013.
3. Pryzdial
ELG, Wright JF. Prothrombinase assembly on an
enveloped virus: evidence that the CMV surface contains procoagulant
phospholipid. Blood 1994; 84 (11):3749-3757.
4. Berg,
D., L. H. Berg, J. Couvaras, and H. Harrison.
"Chronic Fatigue Syndrome And/or Fibromyalgia as a Variation of Antiphospholipid Antibody Syndrome." Blood
Coagulation & Fibrinolysis 10.7 (1999): 435-38. Print.
5. Nicholson AC, Hajjar DP. Herpes
viruses in atherosclerosis and thrombosis: etiologic agents or ubiquitous
bystanders? Arteriosclerosis Thromb Vasc Biol 1998; IS: 339-348.
6. Bordia A, Verma SK, Srivastava KC. Effect
of ginger (Zingiber officinale
Rosc.) and fenugreek (Trigonella
foenumgraecum L.) on blood lipids, blood sugar,
and platelet aggregation ion patients with coronary heart disease. Prostaglandins Leukot Essent Fatty Acids. 1997;56(5):379-384.
7. Nurtjahja-Tjendraputra,
Effie, Alaina J. Ammit,
Basil D. Roufogalis, Van H. Tran, and Colin C. Duke.
"Effective Anti-platelet and COX-1 Enzyme Inhibitors from Pungent
Constituents of Ginger." Thrombosis Research 111.4-5
(2003): 259-65. Print.
8. Teresa Mattiello, Elisabetta Trifirò, Gloria Saccani Jotti, and Fabio M. Pulcinelli. Journal of Medicinal Food. April 2009, 12(2): 334-339.
doi:10.1089/jmf.2007.0640.
9. Robertson,
Virginia. Studies on Papaya Leaf Tea. N.p.: n.p.,
n.d. Print.
10. Maurer,
H.R. "Bromelain: Biochemistry, Pharmacology and Medical Use." Cellular
and Molecular Life Sciences 58.9 (2001): 1234-245. Print.
11. Maurer H. R.,
Eckert K., Grabowska E., Eschmann
K. (2000) Use of bromelain proteases for inhibiting
blood coagulation. Patent WO PCT/EP 98/04406
12. Hsia, Chien-Hsun, Ming-Ching Shen, Jen-Shiou Lin, Yao-Ke Wen, Kai-Lin Hwang, Thau-Ming
Cham, and Nae-Cherng Yang. "Nattokinase
Decreases Plasma Levels of Fibrinogen, Factor VII, and Factor VIII in Human
Subjects☆." Nutrition
Research 29.3 (2009): 190-96. Print.
13. Sumi,
Hiroyuki, Hiroki Hamada, Koichiro Nakanishi, and
Hajime Hiratani. "Enhancement of the
Fibrinolytic Activity in Plasma by Oral Administration of Nattokinases." Acta Haematologica 84.3
(1990): 139-43. Print.
14. Sumi H, Hamada H, Tsushima H, Mihara H. Urokinase-like plasminogen activator increased in plasma after alcohol drinking. Alcohol 1988;23:33-43.